Familial Shar-Pei Fever
By Jeff Vidt, DVM
Familial Shar-Pei Fever (FSF) is a hereditary inflammatory disorder seen in Shar-Pei. It appears to be inherited as an autosomal recessive condition.
Clinical signs: Episodic fever is the most important and consistent clinical sign of this disorder. The tempera-ture commonly is in the 104-107°F (40°C-41.7°C) range. The fever is generally self-limiting lasting 12-36 hours. Another common clinical sign often accompanying the fever is swelling of a joint, usually the hock (tibiotarsal) joint and is known as Swollen Hock Syndrome (SHS). This painful, hot swelling can also involve the carpus (wrist) and the lips and/or muzzle. Dogs with FSF are sick — they are reluctant to move and when they do walk they have a characteristic “walking on eggs” gait. They often are painful in the abdomen and have a characteristic “roached” back. There can be gastrointestinal signs such as mild vomiting and diarrhea as well. These signs are related to synovitis of the affected joint(s), pleuritis and/or peritonitis (inflammation of the lining of the thoracic/abdominal cavity) and the accompanying pain. Along with these clinical signs they are also not eating or drinking.
Pathogenesis: What we do know about this disease is as follows:
- The major function of the immune system is to recognize “SELF” and “NONSELF” and then react appropriately to eliminate the “NON-SELF” antigens. There are two arms of the immune system – INNATE IMMUNITY and ADAPTIVE (HUMORAL) IMMUNITY. The innate immune system is set up to react quickly by generating an inflammatory response. This is initiated by a group of proteins known as PAMPs or Pathogen-Associated Molecular Pattern proteins. The innate immune system is pre-programmed to a respond to a wide variety of environmental triggers. The adaptive immune system is slower in onset and has the advantage that it “remembers” previous encounters. Hence it “learns” and reacts quicker and stronger in future episodes. Both these legs work together to lessen the impact of bacteria, foreign material, viruses, fungi, tumor cells, etc. on the body.
- Inflammation is a normal response in the body and is finely controlled by a “checks and balances” system which regulates the duration and intensity of the response. There are systems in place which turn “ON” the system and turn “OFF” the system to maintain balance.
- A genetic defect in the innate immune system can lead to uncontrolled inflammation resulting in AUTOINFLAMMAORY disease – a syndrome of continuous (constant “ON”) inflammation which is not healthy. A genetic defect in the adaptive immune system leads to an over-reactive immune response resulting in AUTOIMMUNE disease (the body reacting to itself).
- FSF is classified as an AUTOINFLAMMATORY DISORDER due to a genetic mutation in innate immunity and may be the first such described disorder in dogs. There are a number of autoinflammatory diseases described in humans such as Familial Mediterranean Fever, Tumor necrosis factor Receptor – Associated Periodic Syndrome (TRAPS), Cryopyrin – Associated Periodic Syndrome (CAPS) and others. These are lumped together into Hereditary Recurrent Fever Syndromes (HRFS). These are all diseases which are due to mutations in the genes which regulate the production of inflammatory cytokines (chemical messengers) such as those in the interleukin family. FSF dogs are in a constant state of inflammation with high levels of inflammatory proteins such as IL-6, IL-1β, acute phase reactant proteins, and serum amyloid A (SAA) protein, among others. The development of systemic reactive amyloidosis is a potential complication of all the autoinflammatory diseases.
- FSF is more complicated in Shar-Pei due to a genetic mutation which results in Hereditary Cutaneous Hyaluranosis (HCH) – grossly seen as the excessive wrinkles which define the breed. The genetic defect results in over-production of hyaluronan (mucin). Low-molecular weight break down products of hyaluronan metabolism are pro-inflammatory and exacerbate the pro-inflammatory process involved in FSF. Hyaluronan is a normal substance in the body making up the intercellular matrix or scaffolding between cells. Based on its cellular and water content it can present as a free flowing gelatinous material to something as firm as cartilage. Recently a mutation upstream of the HAS2 gene on chromosome13 has been discovered. The mutation is known as the “meatmouth” mutation and is a count number variation (CNV) consisting of multiple copies of a regulatory gene controlling hyaluronan synthesis. Increased levels of hyaluronan are associated with a tendency to develop FSF and amyloidosis. Research is continuing to focus on this mutation in the hope of developing a blood test to determine an individual’s risk of developing FSF +/- amyloidosis.
- The tendency to develop amyloidosis may also represent an additional defect that is probably present throughout the canine genome in all breeds of dogs. Amyloidosis develops in the presence of chronic inflammatory diseases such as heartworm, tuberculosis, systemic fungal diseases, chronic bacterial infections and cancer. FSF and hyaluronosis are built-in triggers for the development of amyloidosis and account for the increased susceptibility of the breed to this complication.
- Pedigree studies indicate that FSF is an inherited disorder in the Shar-Pei probably as an autosomal recessive trait. Survey results have indicated that as many as 23% of Shar-Pei experience fevers of unknown origin. Shar-Pei with FSF have increased levels of the cytokine Interleukin-6 (IL-6). IL-6 is involved with the fever response and is an integral part of triggering the production of Acute Phase Reactant Proteins by the liver. IL-6 is also involved in the Systemic Inflammatory Response Syndrome (SIRS). Dysregulation of IL-6 is the cause of much of the disease in Shar-Pei with FSF. IL-6 also plays a major role in the body’s stress response and serves to “prime” the immune system.
- Shar-Pei with FSF are at risk from early death from systemic amyloidosis. About 5% of the FSF dogs will develop renal failure including renal amyloidosis – a smaller percentage will develop hepatic amyloidosis. This is usually seen in Shar-Pei between the ages of 2-5 years of age. They also seem more susceptible to immune-mediated kidney disease such as membranous glomerulonephritis, protein-losing glomerulopathies, DIC, thromboembolic phenomena such as mesenteric, splenic and pulmonary embolism and Streptococcal Toxic Shock Syndrome (STSS).
- Early on, FSF in Shar-Pei was hypothesized to be an animal model for Familial Mediterranean Fever in humans. Recent work indicates this is not true, although FSF is very similar to FMF in man.
Laboratory Findings: Unfortunately there are no blood tests, etc. which are specific for FSF. During a fever episode there will often be an increased white blood cell count, an increase in liver enzyme levels and other non-specific findings. Work done by Dr. Gary Johnson at the University Of Missouri College Of Veterinary Medicine to develop a DNA blood test to screen for the disease was unsuccessful. The research effort will still continue.
Treatment: It is very important to monitor the temperature in this condition. Initially, fever can be treated using aspirin. Usually a regular strength adult aspirin (325mg) is given every 6- 12 hours for the first 24 hours and then twice a day for 3-5 days thereafter. It is important to continue treatment for several days flowing resolution of the episode to prevent rebound fever. In rare cases where aspirin doesn’t work or for extremely high fevers, dipyrone is given. Other NSAIDs may also be used but response may be a little unpredictable. Some patients will require supportive care with intravenous fluid therapy and in extreme cases emergency treatment similar to heat stroke treatment. Antibiotics are not normally indicated in this condition.
Colchicine: Colchicine is a drug that has been in use in people with FMF to prevent amyloidosis. It is currently being recommended in Shar-Pei with FSF for the same purpose. No studies have been completed to determine if it is useful for this purpose in the Shar-Pei or not. The clinical impression is that it does help. Those dogs on colchicine seem to have fewer FSF episodes and less severe signs while on the drug. Side-effects appear to be minimal at this time. I currently recommend stopping colchicine therapy during an FSF episode while aspirin or other NSAIDs are being used as there is increased risk of gastritis.
Prevention: Shar-Pei with FSF only show symptoms sporadically. It would appear that there are “triggers” involved in initiation of the FSF episodes. One of the major triggers appears to be stress. This may be a dog training class, a dog show, another illness, a dog in heat, excessive exercise, etc. If the owner can recognize these triggers and take steps to avoid them the number of FSF episodes can often be reduced. Diet does not appear to be helpful in prevention of FSF or kidney disease. Surely diet has a role in the management of kidney disease once clinical signs are apparent. Low dose aspirin therapy may be useful in decreasing the incidence of FSF and its severity as well. Aspirin may also be useful as an adjunct therapy in the prevention of thromboembolism.
Monitoring: Monitoring for the complications which often accompany FSF is one of the major goals for the owner of an FSF dog. The primary and most consistent sequela to FSF is kidney failure either due to immune-mediated kidney disease or renal amyloidosis. I currently recommend monitoring a urinalysis every 3 months. The sample should be collected first thing in the morning after the water has been taken up overnight. I primarily look at the urine specific gravity which is a measure of the concentration of the urine and the protein levels in the urine. When the kidneys begin to fail the initial indication is a loss in the ability to produce a concentrated urine. This occurs before there are blood changes related to kidney failure. Increased water consumption, increased urination are the clinical signs associated with a loss of concentrating ability, but these signs are often not recognized. I also think it is wise to do a blood panel every 6-12 months and certainly do one if the urinalysis is abnormal. Weighing your dog periodically is very important. We often don’t recognize a significant weight loss because it is very subtle over a longer period of time. Water consumption and appetite are other important indicators to watch. Amyloidosis is usually medullary in Shar-Pei but can manifest as a protein-losing nephropathy and UPC ratios and treatment with ACE –inhibitors may be necessary.
Complications of FSF: We have already discussed the kidney complications in this condition. Other complications which have been documented include thromboembolism (mesenteric, splenic, pulmonary), DIC (disseminated intravascular coagulation), SIRS (systemic inflammatory response syndrome), MODS (multiple organ dysfunction syndrome), STSS (streptococcal toxic shock syndrome), hypertension associated with renal failure. Many of the deaths following an acute FSF episode are due to these complications. No FSF episode should be treated lightly!
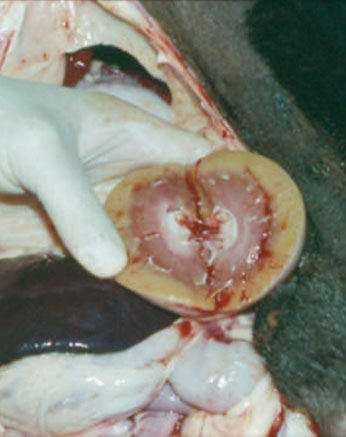
Diagnosis: There is no specific diagnostic test for FSF at this time. Diagnosis is based on the clinical sign of episodic fever in a Shar-Pei. I think every Shar-Pei that dies should be autopsied to determine the cause of death, but this is even more critical in cases involving FSF. Renal amyloidosis can only be diagnosed based on kidney biopsy and staining with Congo Red stain. This stain is specific for the presence of amyloid. Amyloid has been found in other tissues in Shar-Pei as well so special staining should be requested on all tissues submitted for histopathology. Many dogs with FSF will not have amyloid in the tissues at the time the tissues were harvested — this means the absence of amyloid in a biopsy specimen does not mean that dog will not or would not have gone on to develop amyloidosis at a later time. To further confuse the issue, not all Shar-Pei with amyloidosis have shown signs of FSF.
Future: Research is currently underway at the University Of Missouri College Of Veterinary Medicine by Dr. Gary Johnson to develop a DNA blood test. The gene for human FMF was sequenced in the fall of 1997 and with that information Dr. Johnson had hoped to sequence the FSF gene. That information was applied by Dr. Gary Johnson to FSF in a research project founded by the CSPCA Charitable Trust. That project did determine that the mutations causing FMF in man do not exist in FSF in the Shar-Pei; hence they are two distinct, although similar diseases. There are other hereditary inflammatory fever disorders in man and Dr. Kastner at the National Institutes of Health are looking at the disorder with information supplied by Dr. Tintle. Familial Hibernian Fever in man has also been ruled out as the cause of FSF by Dr. Johnson with information supplied by NIH. Work will continue to find the genetic mutation(s) responsible for FSF in Shar-Pei. As of this writing the mutation responsible for FSF has not been found. If a test can be developed, a screening program can be established to screen breeding stock and determine normal individuals, carriers and affected dogs. With this information Shar-Pei breeders can gradually eliminate this genetic disease from the breed. One of the major obstacles to the research revolves around the unpredictable phenotype of FSF. There is no consistent age range when clinical signs develop, the clinical signs can be variable, some dogs develop amyloidosis, some don’t, etc. This makes it very difficult to use genetic selection methods which are based on phenotype.
Recommendations: All Shar-Pei with FSF should be on colchicine and be regularly monitored via urine samples and blood work for development of complications. Dogs with FSF should not be used in breeding programs and should be neutered. Dogs with a family history of FSF should be on colchicine and monitored. Dogs with FSF should be maintained as stress-free as possible.(6/09/09)

(Fig 1.)

Fig.1 shows swelling of the left hock. The hock is erythematosus and very painful. This is known as Swollen Hock Syndrome (SHS) in Shar-Pei circles. This term should only be used in dogs with the fever characteristic for FSF. Other causes of a swollen hock without fever are mucin accumulation (“socks”), allergic reaction, and cellulitis.
Fig.2 shows the characteristic stance of these dogs.


(Fig 3.) This figure illustrates that in less common cases the carpus is affected and rarely there can also be a swollen, painful lip or muzzle.
(Fig. 5) This figure illustrates a kidney affected by amyloidosis.
- Rivas AL, Tintle L, et al: A canine febrile disorder associated with elevated interleukin-6, Clinical Immunol Immunopathol 64:36-45, 1992.
- Tintle, L: Familial Shar-Pei fever and familial amyloidosis of Chinese Shar-Pei dogs:http://www.royalsharpei.com/amyloidosis.htm
- DiBartola SP, et al: Familial renal amyloidosis in Chinese Shar-Pei dogs, J Am Vet Med Assoc204:1212-1216, 1994.
- Olsson M, Meadows JRS, Truvé K, Rosengren Pielberg G, Puppo F, et al. (2011) A Novel Unstable Duplication Upstream of HAS2 Predisposes to a Breed-Defining Skin Phenotype and a Periodic Fever Syndrome in Chinese Shar-Pei Dogs. PLoS Genet 7(3): e1001332.doi:10.1371/journal.pgen.1001332
© Jeff Vidt, DVM (12/2/12)
Dr. Linda Tintle and Dr. Jeff Vidt maintain web sites full of information about the Chinese Shar-Pei. They can be found at www.wvc.vetsuite.com and www.drjwv.com. Dr. Vidt has a “Vets Only Section” of his web site. Vets can click on his link to find instructions on how to get into the area for vets only.